Yejin Kang Explores the Link Between Cholesterol and Muscular Dystrophy
On January 12th, HLI hosted another insightful session in our ongoing Seminar Series. This week, Yejin Kang, a Postdoctoral Fellow at Bernatchez Lab, shared her exciting research on how cholesterol affects muscle health, particularly in the context of muscular dystrophy.
Muscular dystrophy (MD) is a group of genetic conditions that cause muscle weakness and damage. Yejin’s talk, titled The Role of Circulating Cholesterol in Muscular Dystrophy and Muscle Regeneration, explored how changes in cholesterol levels can worsen the effects of this disease and even hinder the body’s ability to repair muscles.

One key takeaway from Yejin’s work is how statin intolerance, a condition that leads to muscle pain, can demonstrate how sensitive muscles are to fluctuations in cholesterol levels. Bernatchez’s lab has been studying the relationship between cholesterol and muscle dysfunction, using pre-clinical models and human samples to uncover new insights. In one experiment, they found that an unhealthy cholesterol level dramatically worsened the condition of mice with muscular dystrophy, leading to severe muscle wasting.
Yejin’s research doesn’t stop at understanding the problem. She is also working on finding better ways to prevent or treat this muscle degeneration by studying how different cholesterol levels impact muscle healing. The team is specifically looking at a group of mice with a genetic mutation similar to one seen in humans with muscular dystrophy, using them to test how cholesterol diets affect muscle regeneration after injury.
Her work is part of a larger effort to understand how metabolic factors like cholesterol can play a role in muscle diseases and could eventually lead to new treatment options.
The seminar was a wonderful opportunity to learn about the real-world impact of cholesterol on muscle health, and Yejin’s contributions to this important area of research are invaluable in the quest for better treatments for muscular dystrophy.
If you want to connect with Yejin and learn more about her work, feel free to visit her ResearchGate profile: https://www.researchgate.net/profile/Yejin-Kang
The Centre for Heart Lung Innovation (HLI) is excited to share that the 2024 Annual Report is now live.
The report highlights major research breakthroughs, new community partnerships, knowledge translation, and trainee accomplishments and activities, capturing the momentum and impact of HLI’s work.
Download the annual report on the right, explore the highlight sections below, or click here for a flip-book view of our report.
2024 Research Snapshot
Click a button to view each graphic.
At the 2025 Heart Centre Nursing Education Day at St. Paul’s Hospital (SPH) and Providence Health Care (PHC), the Bruce McManus Cardiovascular Biobank (BMCB) hosted a Hands-On-Hearts gross anatomy workshop, where cardiac care nurses were offered the rare opportunity to examine human explanted hearts. Participants saw the physical impact of the diseases they treat every day, including the effects of advanced heart failure and implanted devices like the Left Ventricular Assist Device (LVAD).
This year’s theme, Merging History, Best Practice and Compassion in Cardiac Nursing, brought together expert talks, hands-on workshops and opportunities for connection among nursing professionals. Guest speakers covered a range of topics including pregnancy and heart failure, trauma-informed practice, the evolution of cardiac nursing, women’s heart health, and managing heart failure in the context of mental health and substance use disorders.
The BMCB team, including Dr. Gurpreet Singhera, Coco Ng, Tiffany Chang and Viola Tansuma, showed transplant hearts that revealed structural damage caused by cardiomyopathies, ischemic diseases, and end-stage heart failure. Attendees got to observe, feel, and ask questions about how these conditions manifest physically, which are insights not usually available outside of an anatomy lab.
LVAD workshop: Lived experience and hands-on learning
One standout session was the LVAD workshop, led by SPH nurse and patient educators Rachel Milligan and Josie Mackey, and Clinical Nurse Specialist Wynne Chiu. It followed the patient journey from diagnosis to device implantation, featuring stories from LVAD recipients Mike Mclellan and Naomi Lee. The VAD is a life-saving device used in severe, often end-stage heart failure. When the heart becomes too weak to pump blood properly, the LVAD takes over the pumping function, keeping blood circulating through the body.

Mike, who lives with an LVAD, shared what daily life is like with the device, including how he manages battery life and navigates airport security checks. Hearing directly from Mike offered a unique, powerful perspective on the lived experience of VAD patients, highlighting the importance of patient partnership in understanding the realities of care beyond the clinical setting.
Naomi also shared her experiences of living with a VAD for 10 months. Naomi is a second-year nursing student and heart transplant recipient, who received her new heart at age 20. For the biobank team, it was a special moment to reconnect with Naomi. They first met shortly after her transplant, when she visited the biobank to view her own explanted heart.

Since her transplant, Naomi has redirected her professional path from elementary education to healthcare. She now volunteers with organizations such as HeartLife Canada, the Heart and Stroke Foundation of Canada, the Transplant Research Foundation of BC, and BC Transplant. Motivated by the care she received, Naomi hopes to draw from her lived experience as a patient to give back and support others in the healthcare system.
Hands-On Learning with Human Hearts
Later in the day, the BMCB team led the hands-on session and viewing of failed explanted hearts. The session offered cardiac care nurses the rare opportunity to examine hearts affected by conditions such as myocardial infarction, fibrosis and cardiomyopathy, including one specimen with an implanted LVAD. It also highlighted how biobanking of heart tissues plays a critical role in advancing medical research and improves patient care.
For many cardiac care nurses, this was a unique learning opportunity that offered a firsthand look at how the diseases they treat every day appear in the organ itself. The chance to hold and inspect l actual hearts tied together earlier discussions on heart failure and device therapy, offering a full-circle learning experience.

Thank you to the Providence Health Care Heart Centre staff for hosting the valuable event and inviting the biobank to take part in this meaningful day of learning.
Dr. Zachary Laksman has received funding from Genome Canada and Genome BC to lead a project with BC-based Axolotl Biosciences, that will use genomics-informed bio-inks to 3D-print heart tissue. The project aims to improve how scientists study heart disease and test drugs before they reach clinical trials.
Improving heart disease models
Heart disease is a leading cause of death, yet drug development is slow, costly and relies heavily on animal models that do not fully reflect human biology. As a result, many potential drugs fail in clinical trials due to poor early-stage testing models.
3D-printed “cardiac organoids” – small, lab-grown models of heart tissue made from human stem cells – offer a more accurate way to study heart disease and test new drugs.
Two new bio-inks for advancing precision medicine
This project will use human genetic information (“genomics-informed”) to develop two new “bio-inks”: the printing materials that, when combined with stem cells, allow scientists to create functional, realistic heart tissue in the lab. This genomics-informed approach allows researchers to account for biological differences between individuals, including sex-based differences and genetic risk factors.
The first bio-ink, called HeartPrint, will be an application-ready platform that will allow researchers to 3D-print human heart tissue for disease modelling and drug testing.
The second model, HeartPrint-M, will be developed using only stem cells and will include factors that help mimic more mature, adult-like heart tissue. This version will include sex-specific formulations, addressing long-standing gaps in how male and female heart differences are studied in biomedical research.
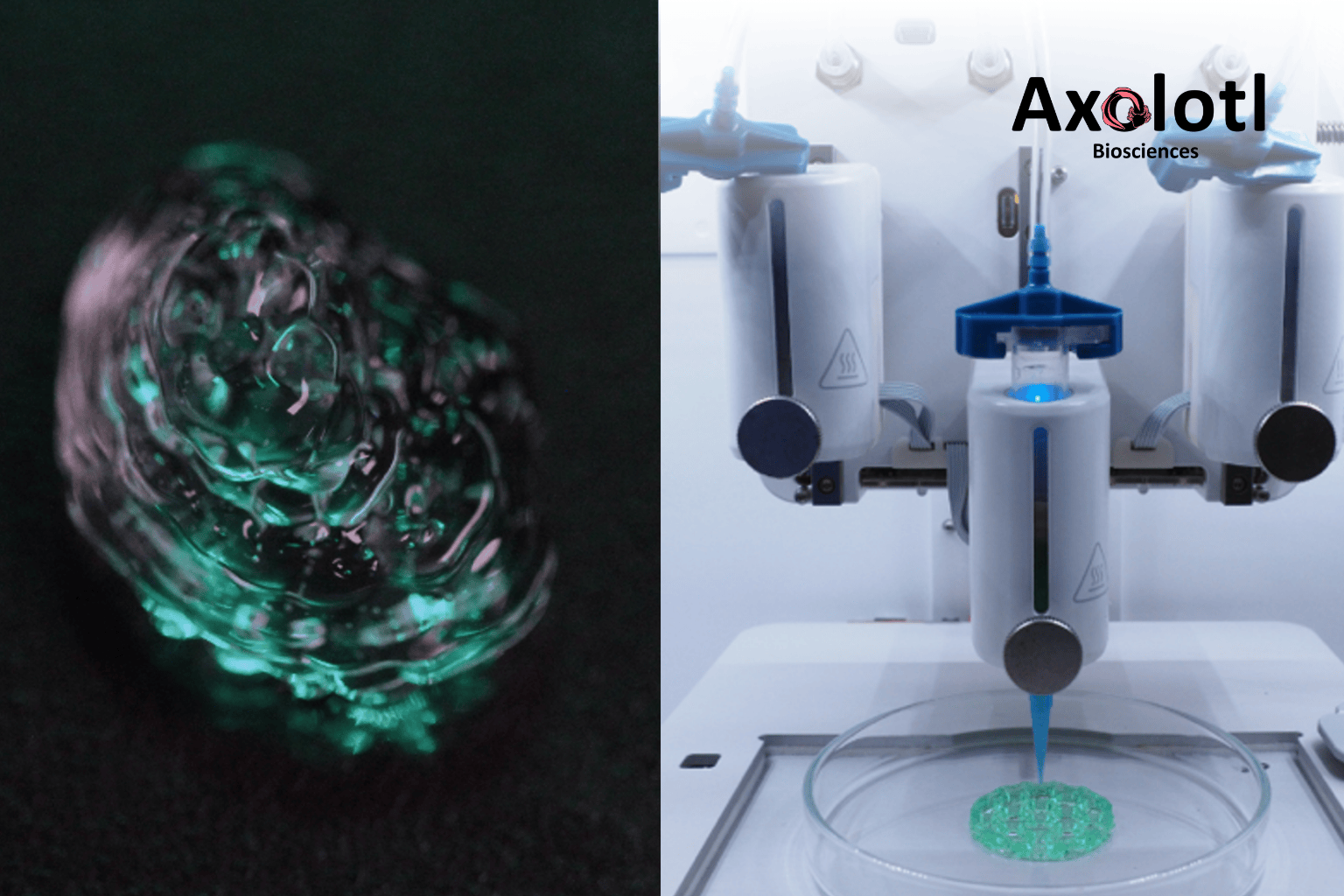
Freshly printed bio-ink (left) is visible. A 3D bioprinter (right) prints bio-ink to create models. Photo courtesy of Axolotl Biosciences.
Led by Dr. Laksman, a principal investigator at HLI, and Dr. Stephanie Willerth, the CEO of Axolotl Biosciences, this project brings together clinical science, bioengineering and genomics. It marks a major step toward safer, faster and more personalized treatment options for heart disease.
The project is being developed in collaboration with Dr. Yuan Yao of HLI and Dr. Leonard Foster of UBC’s Life Sciences Institute. It also receives in-kind support through Michael Smith Health Research BC’s match funding program.
Further Reading
- Read the official project details: Genome Canada – Laksman & Axolotl Biosciences
- Learn more about Axolotl Biosciences: Bioink | Axolotl Biosciences
ABOUT AXOLOTL BIOSCIENCES
Axolotl Biosciences is a Canadian biotechnology start-up based in Victoria, B.C., specializing in 3D bioprinting tools and reagents. The company provides bio-inks and tissue models for use in drug development, disease research and regenerative medicine.
ABOUT DR. ZACHARY LAKSMAN
Dr. Zachary Laksman is a clinician scientist at the University of British Columbia, HLI and St. Paul’s Hospital. His work focuses on cardiac precision medicine through the integration of clinical cardiology, stem cell research, electrophysiology and genomics. His lab is known for developing some of the first “disease-in-a-dish” models for heart conditions, using stem cells to better understand, diagnose and treat cardiac disease.
The Centre for Heart Lung Innovation (HLI) is looking for participants to join the CLOUD Study (Canadian Lung Outcomes in Users of Vaping Devices). Click here to read this post in French.
CLOUD is a multi-year study investigating the effect of vaping on lung health.
Vaping is increasingly popular with both adolescent and adult Canadians, but the long-term health impacts remain unknown. We believe that the tools we currently have to detect lung disease in people who vape may be insufficient and propose new ways to find lung injuries that may impact them over the course of their lives. These include exercise testing, new imaging techniques, and new breathing tests that will demonstrate how vaping may harm their lungs. We will use these tools in both adolescent and adult Canadians to give those who vape important information on the consequences of vaping.
*Please note that interacting with this post (ex, through likes and comments) can identify you with the research, impacting your privacy.
Who can participate in this study?
Adults (Aged 19+)
- Able to provide informed consent.
- At least 19 years of age.
- Fall into one of the following 4 categories:
- You do not smoke or vape
- You only smoke cigarettes
- You only vape
- You smoke cigarettes and vape
- Optional Bronchoscopy and Pulmonary MRI
- Enrolled in the main study
Adolescents (Aged 12-18)
- Able to provide informed consent.
- Aged between 12 years to less than 19 years old.
- Fall into one of the following 2 categories:
- You do not smoke or vape
- You only vape
What will this involve?
- Baseline study visit: Questionnaires, lung function tests, exercise test, blood sample collection, and pulmonary MRI scan (optional for adults).
- Adult-only procedures: Bronchoscopy (optional) and chest CT scan.
- Adolescent-only procedures: Induced sputum sample collection.
- 18 months after baseline: Questionnaires, lung function tests.
- 36 months after baseline: Questionnaires, lung function tests, exercise test, blood sample collection, and pulmonary MRI scan (optional for adults).
- Adult-only procedures: Bronchoscopy (optional) and chest CT scan.
- Adolescent-only procedures: Induced sputum sample collection.
If you would like more information or wish to participate in this study, please visit https://cloudstudy.ca, email respiratory.research@hli.ubc.ca or call 604-806-9465.
PARTICIPATION RÉMUNÉRÉE À UN PROJET DE RECHERCHE : ÉTUDE CLOUD (Canadian Lung Outcomes in Users of Vaping Devices)
CLOUD est une étude pluriannuelle qui s’intéresse aux effets du vapotage sur la santé pulmonaire.
Le vapotage est de plus en plus populaire auprès des jeunes et des adultes canadiens, mais on ne connaît pas ses effets à long terme sur la santé. Nous craignons que les outils dont nous disposons pour détecter les maladies pulmonaires chez les personnes qui pratiquent le vapotage soient insuffisants. C’est pourquoi nous proposons de nouveaux moyens de détecter les lésions pulmonaires qui peuvent les affecter. Il s’agit notamment de tests d’exercice, de nouvelles techniques d’imagerie et de nouveaux tests respiratoires qui démontreront l’effet dommageable du vapotage sur les poumons. Nous utiliserons ces outils autant pour les adolescents que pour les adultes, afin de donner aux vapoteuses et aux vapoteurs d’importantes informations sur les conséquences du vapotage.
*Sachez que l’interaction avec cette publication (par une mention « J’aime » ou un commentaire, par exemple) peut vous identifier, ce qui a un impact sur votre vie privée.
CRITÈRES DE PARTICIPATION
Adultes (19 ans et plus)
- Être en mesure de fournir un consentement éclairé.
- Être âgé(e) d’au moins 19 ans.
- Entrer dans l’une des 4 catégories suivantes :
- Vous ne fumez pas et ne vapotez pas
- Vous ne fumez que la cigarette
- Vous ne faites que vapoter
- Vous fumez la cigarette et vous vapotez
- Bronchoscopie et IRM pulmonaire facultatives
- Personnes inscrites à l’étude principale
Adolescent(e)s (12-18 ans)
- Être en mesure de fournir un consentement éclairé.
- Être âgé(e) de 12 ans à moins de 19 ans.
- Entrer dans l’une des 2 catégories suivantes :
- Vous ne fumez pas et ne vapotez pas
- Vous ne faites que vapoter
Qu’est-ce que la participation implique ?
- Rendez-vous initial: questionnaires, tests de la fonction pulmonaire, test d’effort, prélèvement sanguin et IRM pulmonaire (facultative pour les adultes).
- Interventions réservées aux adultes : Bronchoscopie (facultative) et TDM thoracique.
- Interventions réservées aux adolescents : Collecte d’échantillons d’expectorations induites.
- 18 mois plus tard: questionnaires, tests de la fonction pulmonaire.
- 36 mois après le rendez-vous initial: questionnaires, tests de la fonction pulmonaire, test d’effort, prélèvement sanguin et IRM pulmonaire (facultative pour les adultes).
- Interventions réservées aux adultes : bronchoscopie (facultative) et TDM thoracique.
- Interventions réservées aux adolescents : collecte d’échantillons d’expectorations induites.
Informations et inscriptions : https://cloudstudy.ca ou respiratory.research@hli.ubc.ca ou 604 806-9465.
On this year’s National Indigenous Languages Day (March 31, 2025), we highlight Dr. Pat Camp’s important work in incorporating Indigenous language into culturally safe healthcare and research practices.
Dr. Pat Camp, a Principal Investigator at the Centre for Heart Lung Innovation (HLI), reflects on her research helping people manage chronic lung conditions through exercise, education, and support – a process called pulmonary rehabilitation.
Through collaboration with Carrier Sekani Family Services, Dr. Camp shares how her team is learning to respectfully incorporate Indigenous knowledge into pulmonary rehabilitation research. This includes using the Carrier (Dakelh) language to name body parts—an approach to make pulmonary rehab more culturally safe, respectful, and healing.
“There’s a lot more that we can do”
— Dr. Pat Camp, HLI Principal Investigator
Watch Dr. Pat Camp’s Story
Learn More
Learn about National Indigenous Language Day:
Other links:
New research on low-carb, high-fat diets earns a spot among the five most-read articles in one of cardiology’s leading journals.
A study led by Dr. Iulia Iatan and Dr. Liam Brunham at the Centre for Heart Lung Innovation (HLI) has been recognized as one of JACC: Advances’ Top 5 Most-Read Articles of 2024. Published in one of the most prominent cardiovascular journals, the study’s ranking underscores its impact and the global interest in its findings.
“It is an honour to see our study recognized among the most-read articles in JACC: Advances for 2024. This reflects the growing interest in understanding how dietary choices impact long-term heart health,” said lead author Dr. Iulia Iatan, a clinician-scientist and former postdoctoral fellow at UBC’s Centre for Heart Lung Innovation and the Healthy Heart Program Prevention Clinic at St. Paul’s Hospital.
“To our knowledge, this was one of the first studies to show an association between low-carbohydrate high-fat diets, increased cholesterol, and higher risk of cardiovascular events.”
— Dr. Iulia Iatan, HLI’s former postdoctoral fellow
“I hope these findings encourage both the public and healthcare professionals to consider the long-term effects of these diets, and also inform clinical practice and public awareness on the importance of heart-healthy nutrition.”
Trendy “keto-like” diet under scrutiny
Low-carbohydrate, high-fat (LCHF) diets have gained popularity for various health reasons, including weight loss and diabetes management, but their long-term effects on heart health have been uncertain. This study found that “keto-like” diets are linked to higher cholesterol levels and a twofold increase in major heart problems, including heart attacks and strokes over the next decade. The risk was highest for those with a genetic predisposition to high cholesterol.
To investigate this link, Dr. Iatan and the team analyzed data from the UK Biobank, tracking 305 participants who followed an LCHF diet—defined as <25% of daily calories from carbohydrates and >45% from fat—over an average of 12 years. They examined lipid levels and cardiovascular events, comparing outcomes to those on normal, standard diets.
A further finding from the study was that the risk of severely elevated cholesterol was highest among those individuals with an elevated polygenic risk score, suggesting a genetic predisposition to diet-induced increases in cholesterol in some people.
These findings emphasize the need for caution among followers of this dietary pattern, especially for those with high cholesterol or a personal or family history of heart disease.
What’s next?
Dr. Brunham and colleagues plan to continue examining how genetic differences influence response to various dietary patterns and their effects on heart health. Future research will also explore whether genetic testing can help create more personalized dietary recommendations and improve understanding of variations between individuals in response to different diets.
A big moment for HLI
This recognition reinforces HLI’s leadership in cardiovascular research and its role in providing strong, evidence-based guidance on health and disease prevention. With this study ranking among JACC: Advances’ most-read of the year, HLI continues to drive research that informs medical practice and public health.
“This is a great recognition of the quality of cardiovascular research taking place at HLI and our centre’s leadership in the field of lipid disorders.”
— Dr. Liam Brunham, HLI’s principal investigator
Further Reading
- Read the full study: JACC: Advances
- Check out Dr. Iulia Iatan’s CNN feature: CNN News Video
- Watch the 3-minute summary by Dr. Liam Brunham: PACE-CME Video
Media Coverage
Read our previous article on this study: ‘Keto-Like’ Diet May be Linked to Increased Risk of Heart Disease
Two HLI lung health researchers are being recognized with a prestigious national award.

Congratulations to HLI principal investigators, Dr. Pat Camp and Dr. Christopher Carlsten, who have been honoured with the King Charles III Coronation Medal—a national recognition of their contributions to Canada and the community.
This award, the first commemorative medal marking the coronation of His Majesty King Charles III on May 6, 2023, celebrates individuals who have made a significant impact in Canada. Recipients are recognized for their work in areas that reflect values shared by both King Charles III and Canadians, including service, environment and sustainability, and diversity.
- Dr. Camp is breaking down barriers to lung health care. As a physical therapist and researcher, her work focuses on making pulmonary rehabilitation and physical activity programs more accessible, particularly for people in rural and First Nations communities. By working directly with these communities, she helps co-design programs that reflect their needs and ensure their voices are heard.
- Dr. Carlsten is exposing the dangers in the air we breathe. His research focuses on how air pollutants, like diesel exhaust, harm lung health over time, working to better understand the risks of breathing in polluted air at work or in the environment. As a clinician-scientist, he treats patients affected by workplace and environmental toxins, translating research into real-world care.
Drs. Camp and Carlsten are among 39 distinguished Canadians nominated by the Canadian Lung Association (CLA) for their outstanding contributions to respiratory health research. In British Columbia, they are two of just three recipients of this national honour.
Congratulations again to Dr. Camp and Dr. Carlsten on this well-deserved recognition!
Read More
Connect
- Dr. Pat Camp on X (Twitter): @UBCPulmRehabRes
- Dr. Christopher Carlsten’s Lab