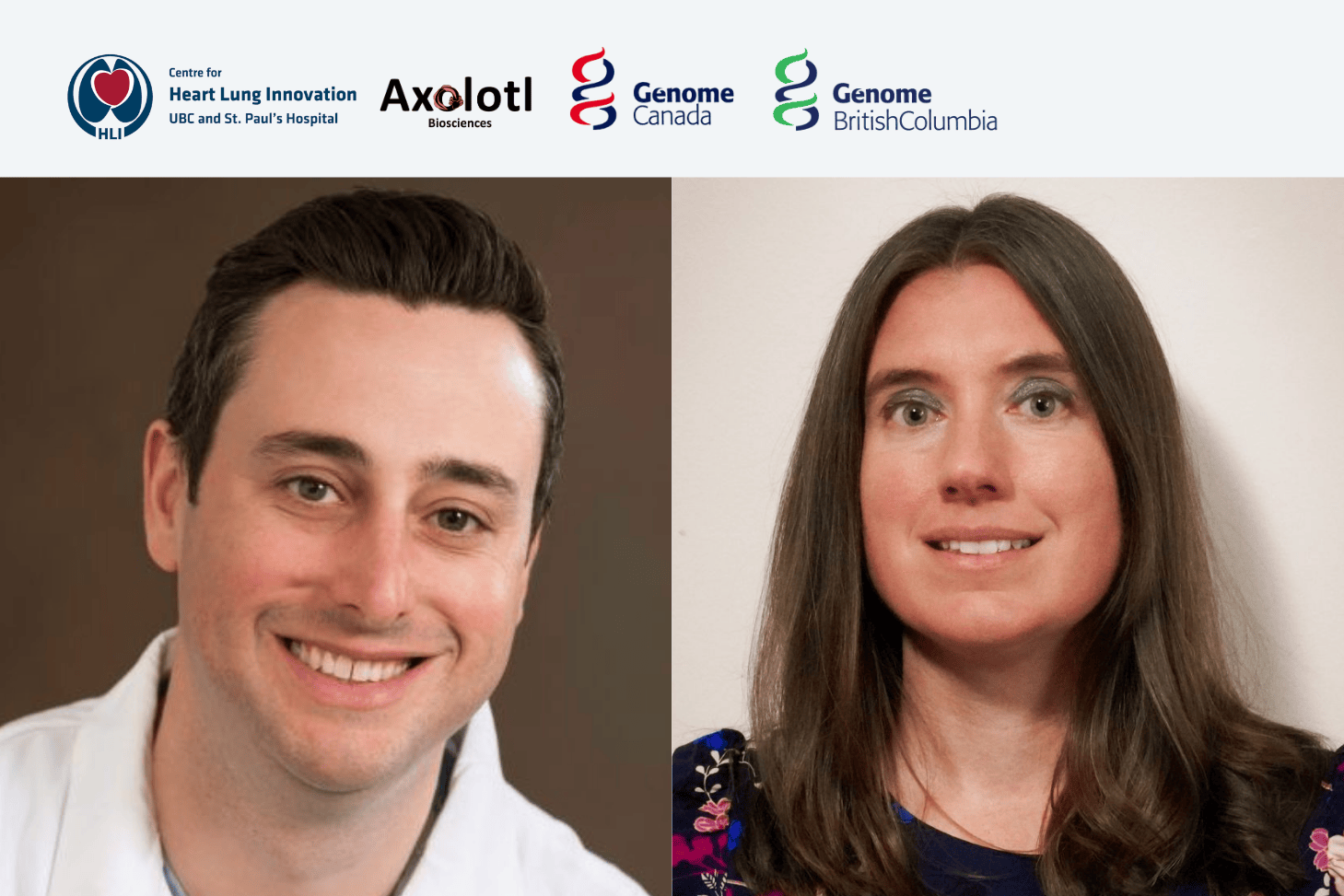
HLI is proud to celebrate the success of Dr. Janice Leung and Dr. Scott Tebbutt, who along with their co-applicants and research teams, have received over $1.8 million in funding from the Canadian Institutes of Health Research (CIHR) Fall 2025 Project Grant competition. This funding will support important new research aimed at improving care for people living with lung disease, heart transplants, and health inequities across Canada.

Understanding COPD Beyond Smoking
Dr. Janice Leung will lead the MAPLE-SEED Study, a project focused on understanding why some people develop chronic obstructive pulmonary disease (COPD) even though they have never smoked. COPD is a long-term lung disease that affects breathing and impacts more than 2.6 million Canadians.
While smoking is a major cause of COPD, it does not explain all cases. About one in five people with COPD have never smoked, suggesting other factors play an important role. Dr. Leung’s research looks at how life experiences and living conditions such as childhood hardship, income level, education, air pollution, diet, and neighbourhood environment can affect lung health over time.
The study focuses on changes in the body that occur at the molecular level, specifically through a process called DNA methylation. In simple terms, DNA methylation acts like a biological record of the experiences a person has had throughout their life. These changes can also reflect how quickly the body is aging, sometimes referred to as a “biological clock.”
Dr. Leung’s team hypothesizes that long-term exposure to social and environmental challenges speeds up biological aging and increases the risk of COPD and poor breathing outcomes.
Using information from two large Canadian studies that follow people over many years, the research will:
- Explore how life circumstances and resulting changes in DNA methylation affect lung health
- Identify risk factors for biological aging and COPD – and potentially ways to improve prevention and treatment
In the long term, the applicants hope that this work leads to the development of a simple blood test to help identify people at higher risk of worsening lung disease.
This research brings together experts from many fields, including lung medicine, public health, biology, and data science. The goal is to help prevent COPD, improve early detection, and reduce health disparities.
Improving Early Detection of Complications After Heart Transplantation
Dr. Scott Tebbutt’s research project focuses on improving care for people who have received a heart transplant. Over time, many transplant recipients develop a condition called cardiac allograft vasculopathy (CAV), which causes the blood vessels of the transplanted heart to narrow. CAV is the leading cause of late transplant failure.
Currently, CAV is usually detected through invasive heart tests, often only after symptoms appear. Dr. Tebbutt’s team aims to develop a simple blood test that can detect signs of CAV much earlier, before serious damage occurs.
The research will look for small changes in the blood such as proteins and molecules that signal early injury or inflammation in the heart. By studying blood samples collected at different times after transplantation, the team hopes to identify patterns that clearly separate healthy recovery from early disease.
This research project will:
- Identify early warning signs of CAV using blood samples
- Track how these signals change over time in transplant patients
- Test how accurately these blood markers can predict disease
- Combine multiple blood signals into a reliable early-detection tool
Led by Dr. Tebbutt and Co-Applicant and HLI Research Associate Dr. Chengliang Yang, the long-term goal of this research is to improve monitoring, reduce invasive testing, and help patients receive treatment sooner.
Making Research Matter for Patients
Together, these CIHR-funded projects reflect HLI’s commitment to research that puts patients first. By studying how social conditions affect lung disease and by developing earlier, less invasive tests for heart transplant complications, these projects aim to improve quality of life, reduce health disparities, and support better outcomes for patients across Canada.
Congratulations to Dr. Leung, Dr. Tebbutt, and their research teams and co-applicants on being awarded these project grants.
Dr. Zachary Laksman has received funding from Genome Canada and Genome BC to lead a project with BC-based Axolotl Biosciences, that will use genomics-informed bio-inks to 3D-print heart tissue. The project aims to improve how scientists study heart disease and test drugs before they reach clinical trials.
Improving heart disease models
Heart disease is a leading cause of death, yet drug development is slow, costly and relies heavily on animal models that do not fully reflect human biology. As a result, many potential drugs fail in clinical trials due to poor early-stage testing models.
3D-printed “cardiac organoids” – small, lab-grown models of heart tissue made from human stem cells – offer a more accurate way to study heart disease and test new drugs.
Two new bio-inks for advancing precision medicine
This project will use human genetic information (“genomics-informed”) to develop two new “bio-inks”: the printing materials that, when combined with stem cells, allow scientists to create functional, realistic heart tissue in the lab. This genomics-informed approach allows researchers to account for biological differences between individuals, including sex-based differences and genetic risk factors.
The first bio-ink, called HeartPrint, will be an application-ready platform that will allow researchers to 3D-print human heart tissue for disease modelling and drug testing.
The second model, HeartPrint-M, will be developed using only stem cells and will include factors that help mimic more mature, adult-like heart tissue. This version will include sex-specific formulations, addressing long-standing gaps in how male and female heart differences are studied in biomedical research.
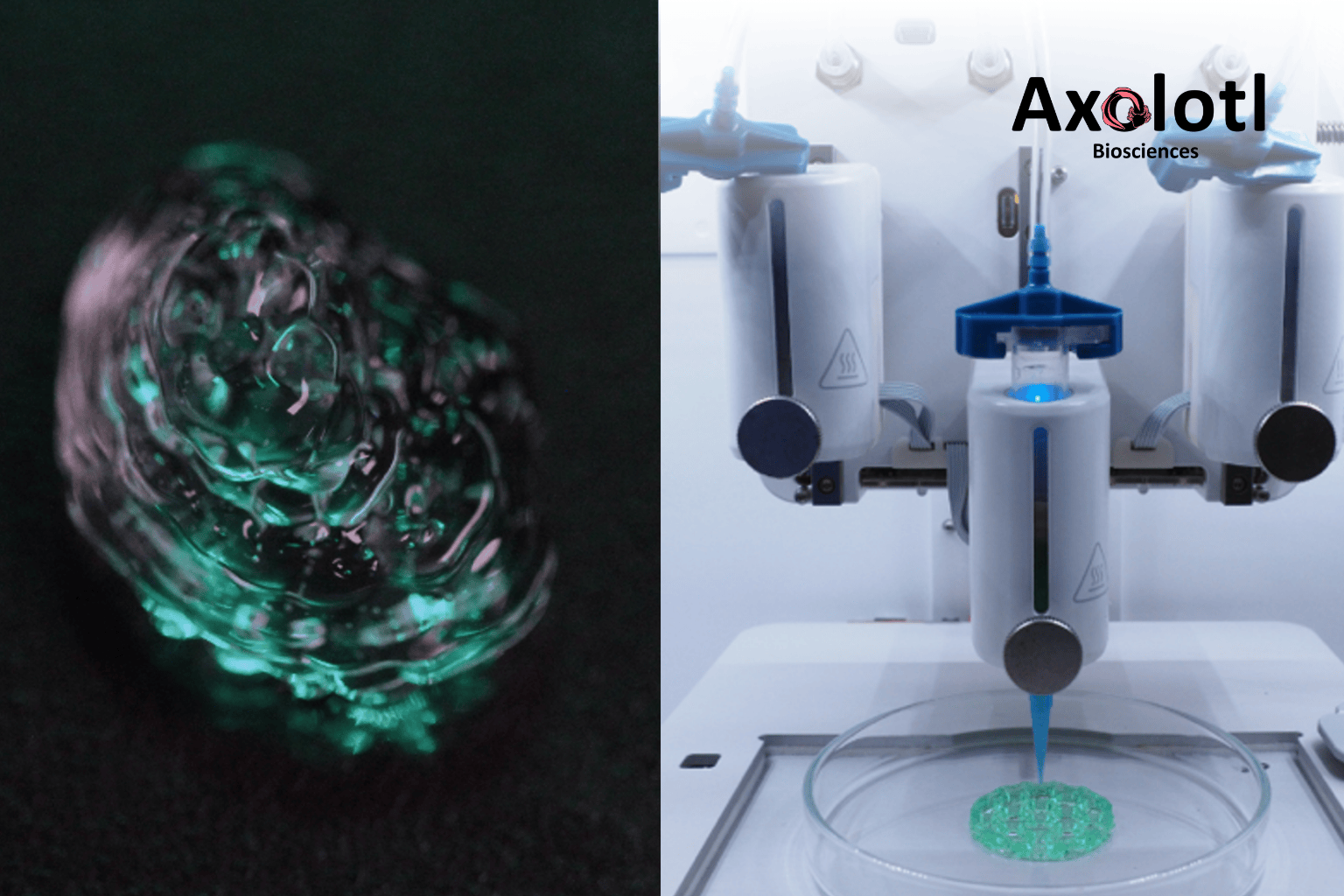
Freshly printed bio-ink (left) is visible. A 3D bioprinter (right) prints bio-ink to create models. Photo courtesy of Axolotl Biosciences.
Led by Dr. Laksman, a principal investigator at HLI, and Dr. Stephanie Willerth, the CEO of Axolotl Biosciences, this project brings together clinical science, bioengineering and genomics. It marks a major step toward safer, faster and more personalized treatment options for heart disease.
The project is being developed in collaboration with Dr. Yuan Yao of HLI and Dr. Leonard Foster of UBC’s Life Sciences Institute. It also receives in-kind support through Michael Smith Health Research BC’s match funding program.
Further Reading
- Read the official project details: Genome Canada – Laksman & Axolotl Biosciences
- Learn more about Axolotl Biosciences: Bioink | Axolotl Biosciences
ABOUT AXOLOTL BIOSCIENCES
Axolotl Biosciences is a Canadian biotechnology start-up based in Victoria, B.C., specializing in 3D bioprinting tools and reagents. The company provides bio-inks and tissue models for use in drug development, disease research and regenerative medicine.
ABOUT DR. ZACHARY LAKSMAN
Dr. Zachary Laksman is a clinician scientist at the University of British Columbia, HLI and St. Paul’s Hospital. His work focuses on cardiac precision medicine through the integration of clinical cardiology, stem cell research, electrophysiology and genomics. His lab is known for developing some of the first “disease-in-a-dish” models for heart conditions, using stem cells to better understand, diagnose and treat cardiac disease.
HLI researchers receive over $1.86 million from CIHR’s Fall 2024 Project Grant competition.
The Centre for Heart Lung Innovation (HLI) is proud to celebrate the achievements of 3 principal investigators who have been awarded funding through the Canadian Institutes of Health Research (CIHR) Project Grants, Fall 2024 competition. This funding will drive innovative research in cardiovascular health, infection and immunity, and transplant medicine, advancing scientific discovery and improving patient outcomes.

Congratulations to the following recipients:
Dr. Scott Tebbutt – $229,500
Metabolomic biomarkers for early detection of acute cellular rejection in heart transplant recipients (HLI Co-investigator: Dr. Chengliang Yang) – CIHR Link
For people with severe heart failure, heart transplantation is a life-saving surgery. However, the body’s immune system may attack the new heart in a condition called acute cellular rejection (ACR). Currently, detecting ACR requires invasive biopsies.
Dr. Scott Tebbutt and HLI Co-investigator Dr. Chengliang Yang are looking into non-invasive blood tests to identify ACR after patients undergo a heart transplant surgery. The development of this test could help doctors quickly identify and treat rejection, improving the health of heart transplant recipients.
Dr. James A. Russell – $719,101
Development of Lipid nanoparticle RNA systems as novel therapeutics for endotoxemia resulting from severe bacterial infections – CIHR Link
Severe bacterial infections, which can lead to pneumonia and sepsis, are leading causes of death worldwide. While antibiotics are essential, some bacteria develop resistance (“superbugs”), making infections harder to treat.
Dr. James A. Russell’s team is developing RNA-based drugs that work by blocking harmful genes or boosting the body’s defenses during infections. These next-generation drugs delivered using lipid nanoparticles, a safe delivery vehicle, could enhance the body’s ability to fight infections, working alongside antibiotics to improve treatment outcomes.
As a commercialization grant, inventions can be patented (IP) and then transferred (“licensed”) to a company called Resolve Nanotherapeutics, that will drive clinical development of these urgently-needed drugs for severe infections.
Dr. Pascal Bernatchez – $914,175
Activation of the chronic endothelial function reserve for the prevention and regression of aortopathies (HLI Co-investigator: Dr. Scott Tebbutt) – CIHR Link
Aortopathies are a group of diseases that affect the aorta, the largest blood vessel in the body. These conditions can weaken the aorta’s walls, increasing the risk of life-threatening conditions like tears and aneurysms (ballooning of the vessel). While patients are often given medication to lower blood pressure to reduce the damage, these treatments do not always stop the disease from progressing.
Dr. Pascal Bernatchez and HLI co-investigator Dr. Scott Tebbutt are researching how to activate natural defenses of blood vessels to improve vessel health in aortopathies. Their previous studies suggest that increasing nitric oxide levels—a chemical released naturally in response to blood flow—may better protect blood vessels. They aim to study this further and are also working to develop blood biomarkers that can indicate whether a patient’s treatment is effective. This approach would offer a more precise way to monitor and personalize care.
We congratulate all the awardees on this well-deserved recognition and look forward to seeing their contributions to advancing health research.