New research from the Centre for Heart Lung Innovation (HLI) has identified inflammation in the lungs’ smallest airways as the cause of pulmonary long COVID-19.
A research team led by the HLI’s Director, Dr. Don Sin, used xenon MRI, an advanced imaging technology, and single-cell sequencing of lung samples, supported by the HLI’s biobank team, to uncover the underlying mechanism behind persistent respiratory symptoms in long COVID patients. These findings were published in three articles in the European Respiratory Journal.

What is long COVID?
Five years on from the beginning of the COVID-19 pandemic, many COVID patients continue to be impacted by residual symptoms lingering after the initial illness, a condition known as long COVID. Affecting approximately 10 per cent of people infected with COVID-19, long COVID is a multi-system disorder with diverse presentations, including brain fog, fatigue, joint pain, shortness of breath, wheeziness, and cough. These symptoms can significantly impact patients’ quality of life and are associated with increased health care costs.
The HLI research team focused on identifying the cause of pulmonary long COVID, which presents with persistent lung symptoms and accounts for approximately one-third of long COVID cases.
Detailed lung scans made possible with xenon MRI
Despite experiencing often-debilitating symptoms, 80 to 90 per cent of the long COVID participants tested by the HLI team showed normal results on standard lung function tests and CT scans.
“I distinctly remember a nurse who could no longer work after recovering from acute COVID. He had so much shortness of breath, even with just minimal exertion, that he had to go on long-term disability. And yet, his breathing test was normal. His CT scan was also normal,” says Dr. Sin.
The researchers suspected that these standard tests were not sensitive enough to detect the root cause of these symptoms, and so they turned to hyperpolarized xenon gas magnetic resonance imaging (xenon MRI), an advanced method that enables three-dimensional imaging of lung function.
In 2019, with support from St. Paul’s Foundation and the Canada Foundation for Innovation, St. Paul’s Hospital obtained a specialized MRI and hyperpolarizer. Together, these devices enabled the use of inhaled hyperpolarized xenon gas to image the lungs’ airways and track the flow of oxygen into the bloodstream, a process known as gas exchange. Hyperpolarization enhances the xenon’s magnetism, making it more visible to the MRI.
“It’s particularly the gas exchange component that makes xenon MRI so unique,” says Dr. Rachel Eddy, Director of the HLI’s MRI core who launched the centre’s xenon MRI research program. As xenon follows the same gas-transfer pathways as oxygen, xenon MRI is able to image the separate components of gas exchange, allowing researchers to identify where in the lungs a problem is occurring.
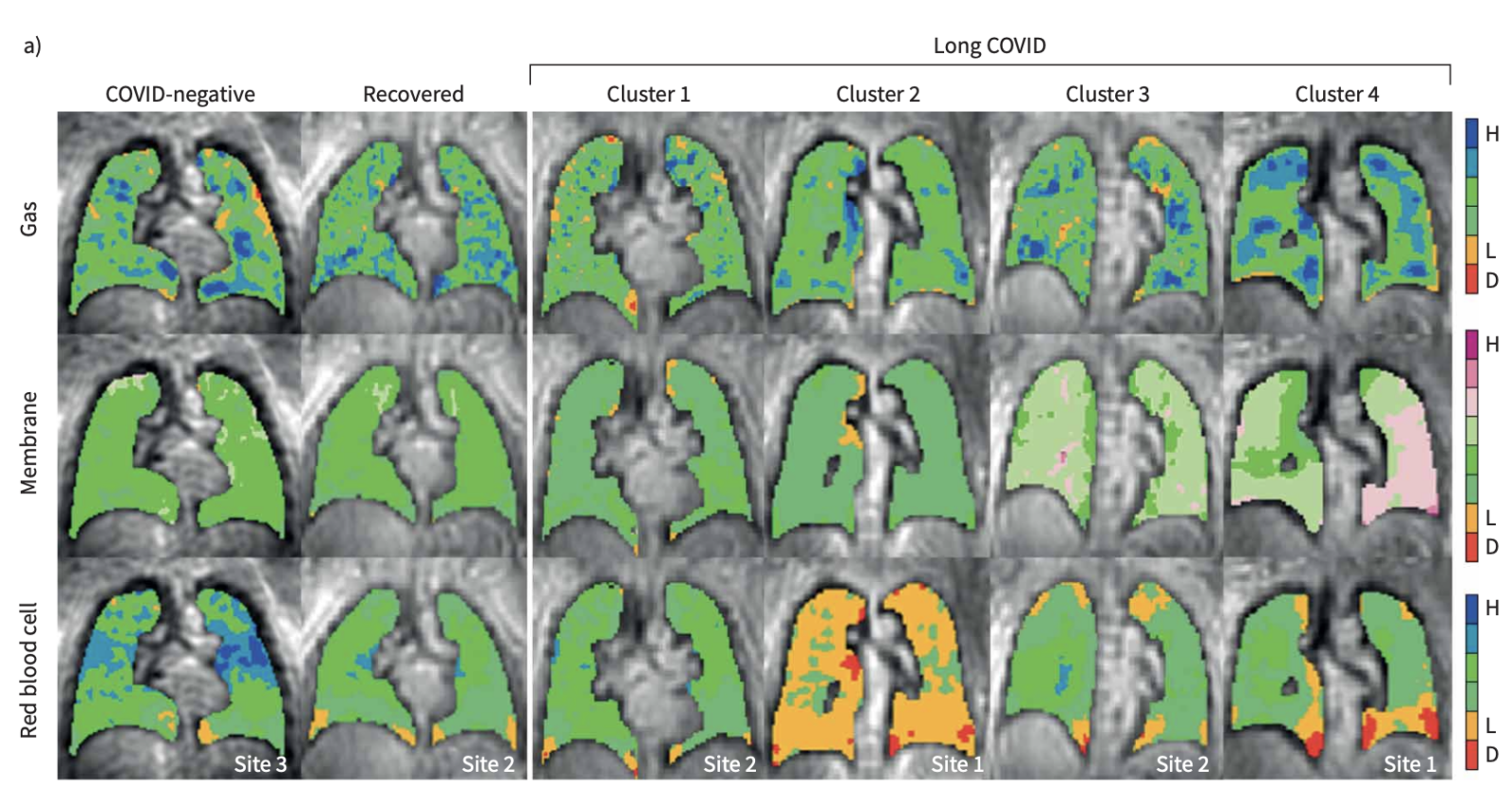
By analyzing combined data from the HLI, Duke University, and the University of Kansas Medical Centre from xenon MRI scans of a large cohort of long COVID patients, the researchers identified four clusters, or subgroups, of pulmonary long COVID, which were characterized by different types of gas exchange abnormalities.
The researchers determined that pulmonary long COVID is primarily driven by gas exchange problems in the small airways, where oxygen enters the bloodstream, which cannot be visualized in traditional scans or lung function tests.
“That’s what hyperpolarized xenon gas MRI does. It lets us see beneath the surface,” says Dr. Sin.
Single-cell profiling identified inflammation in small airways
To determine the cellular and molecular drivers of these abnormalities, a subset of patients who had participated in the xenon MRI study underwent bronchoscopies to take tissue samples from their small airways, which were analyzed with single-cell RNA sequencing.
Because single-cell sequencing requires fresh, living tissue, the research team faced logistical challenges in transporting the samples from St. Paul’s Hospital to the University of British Columbia, where the sequencing equipment is located. To ensure the cells survived the journey, they utilized the expertise of the HLI biobanking team to process and prepare the samples.
“The biobanking facility is much more than just keeping things in the freezer. It’s actually developing protocols and methods to enable the use of human volunteer tissues for research,” says Dr. Sin. The HLI is home to several influential biobanks, including the James Hogg Lung Biobank and the Bruce McManus Cardiovascular Biobank.
The single-cell sequencing found that the pulmonary long COVID patients had neutrophilic inflammation in the small airways. Neutrophils, immune cells that normally help fight infection, were continuing to trigger an immune response, even though the virus was gone.
“They’re like dirty bombs. They come in to kill the bacteria or viruses,” says Dr. Sin. “Once all the pathogens are killed off, then the body should shut down the recruitment of these cells into the small airways.” In pulmonary long COVID patients, these cells remain, causing damage to the small airways and driving the symptoms of pulmonary long COVID.
Inflammation is likely to resolve
A few key questions remain, such as why some people develop long COVID while others recover fully. It is still unknown why these inflammatory cells persist, or if this phenomenon could occur with other viruses like influenza or RSV.
“We don’t think this is specific to coronavirus. If a virus gets in deep enough into your airways, we think that this can trigger, in some individuals, a persistent response for a period of time,” says Dr. Sin.
Encouragingly for pulmonary long COVID patients, Dr. Sin and his team believe that this inflammation, which is relatively mild, will likely resolve on its own over time, provided it isn’t exacerbated by factors like smoking, exposure to wildfire smoke, or additional COVID-19 infections.
“Prevention, breathing in clean air, refraining from smoking and dusty environments, those are, I think, very important preventative measures. If patients keep on doing that, over time we think this inflammation will settle on its own,”
— Dr. Don Sin, HLI Director
Read more
- Cluster analysis to identify long COVID phenotypes using 129Xe magnetic resonance imaging: a multicentre evaluation
- Single-cell sequencing reveals cellular landscape alterations in the airway mucosa of patients with pulmonary long COVID
- A proposed approach to pulmonary long COVID: a viewpoint
This article was originally written by Grace Jenkins and published on March 24, 2025 through Providence Research. Read the article on Providence Research here.
New research on low-carb, high-fat diets earns a spot among the five most-read articles in one of cardiology’s leading journals.
A study led by Dr. Iulia Iatan and Dr. Liam Brunham at the Centre for Heart Lung Innovation (HLI) has been recognized as one of JACC: Advances’ Top 5 Most-Read Articles of 2024. Published in one of the most prominent cardiovascular journals, the study’s ranking underscores its impact and the global interest in its findings.
“It is an honour to see our study recognized among the most-read articles in JACC: Advances for 2024. This reflects the growing interest in understanding how dietary choices impact long-term heart health,” said lead author Dr. Iulia Iatan, a clinician-scientist and former postdoctoral fellow at UBC’s Centre for Heart Lung Innovation and the Healthy Heart Program Prevention Clinic at St. Paul’s Hospital.
“To our knowledge, this was one of the first studies to show an association between low-carbohydrate high-fat diets, increased cholesterol, and higher risk of cardiovascular events.”
— Dr. Iulia Iatan, HLI’s former postdoctoral fellow
“I hope these findings encourage both the public and healthcare professionals to consider the long-term effects of these diets, and also inform clinical practice and public awareness on the importance of heart-healthy nutrition.”
Trendy “keto-like” diet under scrutiny
Low-carbohydrate, high-fat (LCHF) diets have gained popularity for various health reasons, including weight loss and diabetes management, but their long-term effects on heart health have been uncertain. This study found that “keto-like” diets are linked to higher cholesterol levels and a twofold increase in major heart problems, including heart attacks and strokes over the next decade. The risk was highest for those with a genetic predisposition to high cholesterol.
To investigate this link, Dr. Iatan and the team analyzed data from the UK Biobank, tracking 305 participants who followed an LCHF diet—defined as <25% of daily calories from carbohydrates and >45% from fat—over an average of 12 years. They examined lipid levels and cardiovascular events, comparing outcomes to those on normal, standard diets.
A further finding from the study was that the risk of severely elevated cholesterol was highest among those individuals with an elevated polygenic risk score, suggesting a genetic predisposition to diet-induced increases in cholesterol in some people.
These findings emphasize the need for caution among followers of this dietary pattern, especially for those with high cholesterol or a personal or family history of heart disease.
What’s next?
Dr. Brunham and colleagues plan to continue examining how genetic differences influence response to various dietary patterns and their effects on heart health. Future research will also explore whether genetic testing can help create more personalized dietary recommendations and improve understanding of variations between individuals in response to different diets.
A big moment for HLI
This recognition reinforces HLI’s leadership in cardiovascular research and its role in providing strong, evidence-based guidance on health and disease prevention. With this study ranking among JACC: Advances’ most-read of the year, HLI continues to drive research that informs medical practice and public health.
“This is a great recognition of the quality of cardiovascular research taking place at HLI and our centre’s leadership in the field of lipid disorders.”
— Dr. Liam Brunham, HLI’s principal investigator
Further Reading
- Read the full study: JACC: Advances
- Check out Dr. Iulia Iatan’s CNN feature: CNN News Video
- Watch the 3-minute summary by Dr. Liam Brunham: PACE-CME Video
Media Coverage
Read our previous article on this study: ‘Keto-Like’ Diet May be Linked to Increased Risk of Heart Disease