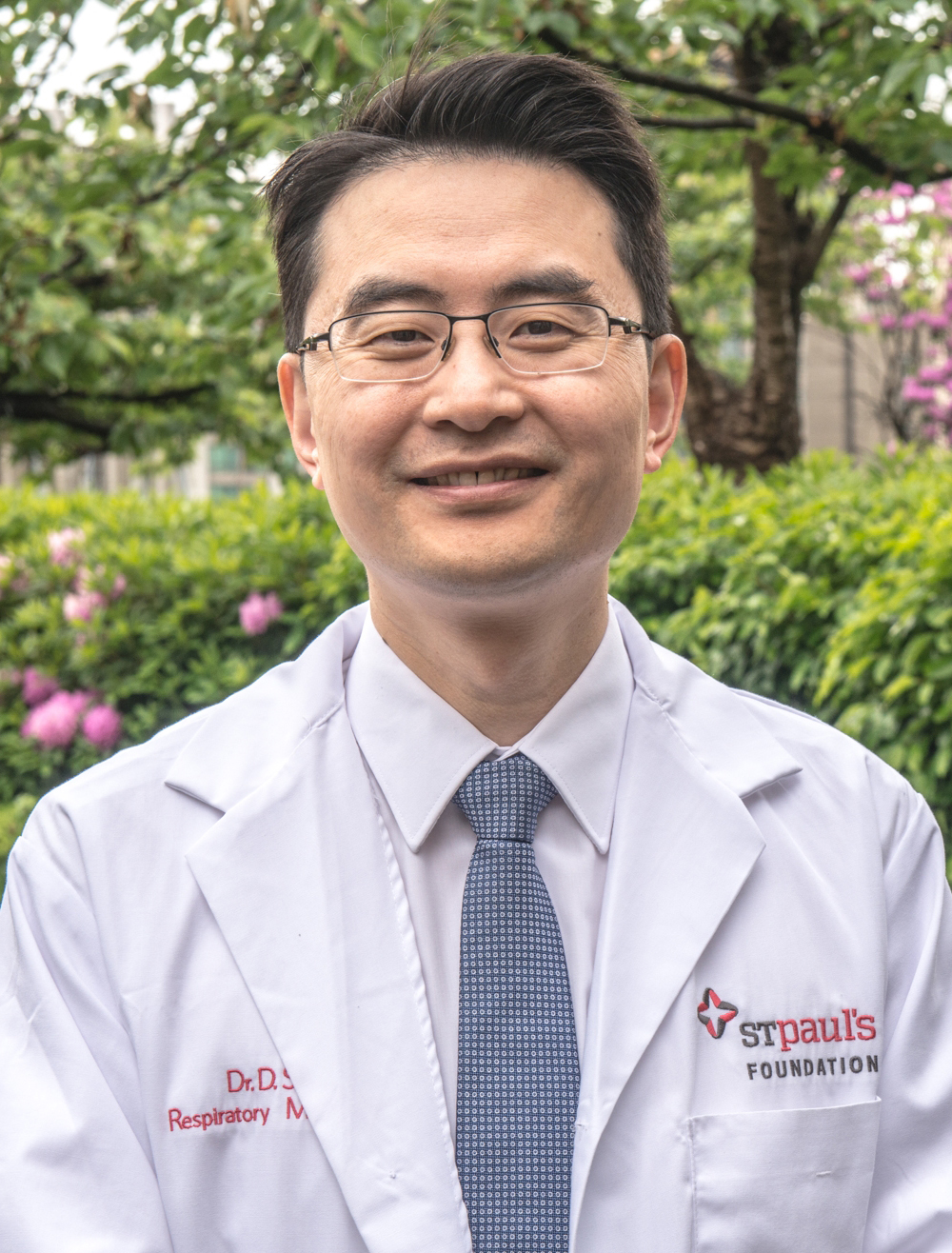
Dr. Don Sin
ProfessorAbout
Don Sin is the Director of the Centre for Heart Lung Innovation (HLI), a Professor of Medicine at University of British Columbia (UBC) and respirologist at St. Paul’s Hospital (SPH). He holds a Tier 1 Canada Research Chair in COPD and the De Lazzari Family Chair at HLI. He has published 700 peer-reviewed papers and has an H-index of 110. He obtained his medical degree at University of Alberta in 1991. He currently serves on the Global initiative for chronic Obstructive Lung Disease (GOLD) scientific committee and CTS COPD guidelines committee and is the deputy chief editor for the European Respiratory Journal. His research focus is using “omics” data to discover novel biomarkers of disease activity and new therapeutic targets to reduce hospitalization and mortality in patients with COPD.
Education & Training
- University of Alberta, MD (1991)
- Harvard University, MPH (1997)
Area of Interest
Because COPD is a heterogeneous disorder, large sample sizes are generally required for therapeutic and even mechanistic studies to enable sufficient statistical power. This problem is exacerbated by the fact that even within a given COPD lung, there is tremendous variability in the severity and extent of the disease.
With the advent of in vivo imaging techniques such as high-resolution CT scans and more recently functional magnetic resonance imaging (MRI), structural abnormalities and disease activity levels can be detected and mapped out regionally prior to sampling of small airways, which are the primary site of disease in COPD (e.g. sampling can be done using bronchoscopy). By knowing which regions of the lung are “hot” and which are “quiescent” a priori, bronchoscopists can take samples in a targeted way to ensure that the full spectrum of disease activity is represented in the sampling process and more importantly, that there is alignment of histologic, molecular and microbial changes in these samples with the disease activity readouts from in vivo imaging.
Over the next 7 years, we will optimize the use of hyperpolarized 129Xe MRI imaging for COPD. In the same subjects, we will also perform research bronchoscopies and sample different small airways based on disease activity readouts from the in vivo imaging. We will then perform multi-omics evaluation of bronchoscopic brushes (which are >95% pure epithelial cells) and bronchoalveolar lavage fluid (BALF). The multi-omic evaluation will include: 1) 16S sequencing for the microbiome; 2) bulk RNA-seq (and single cell seq for sub-projects); 3) DNA methylation and other epigenetic interrogations; and others. The cellular components of BALF are >80% macrophages, which can be profiled, and the supernatant can be used to evaluate surfactants, cytokines/growth factors and other molecules that may play an important role in COPD pathogenesis. Examples of projects include:
1. Phenotyping of alveolar macrophages in COPD across disease spectrum. Currently, little is known about the role of macrophages in COPD pathogenesis despite the fact that >80% of the cellular content in BALF are macrophages. Preliminary work in our lab indicates that dissimilar to healthy control subjects where a majority of alveolar macrophages demonstrate classic M1 or M2 surface markers, macrophages in COPD BALF cannot be phenotyped into these categories. We will perform single cell sequencing and use flow cytometry to characterize the alveolar macrophages in COPD patients versus healthy controls and determine the origin of these “COPD” macrophages (ie. tissue resident versus monocyte-derived) and their functional responses (e.g. phagocytosis, migration, chemokine production, etc.). Importantly, we will relate the presence of these macrophages to important clinical outcomes such as risk of exacerbation in these patients.
2. Evaluation of airway dysbiosis and host inflammatory responses in COPD airways. We have shown previously that airway dysbiosis relates significantly to poor outcomes in COPD patients including mortality. Using the multi-omics and imaging technology platforms in the lab, we will determine whether the airway microbiome within a lung changes depending on the disease severity readouts of MRI and CT scans. We postulate that areas with poor function (i.e. more emphysema and greater hypoxia) will demonstrate a significantly different microbiome (compared with less hypoxic regions) and the microbiome will modify the host’s genomic/inflammatory responses in these airways. We will then test the hypothesis that drugs that modulate regional hypoxia will modify the microbiome as well as the host’s immune response.
Team Members
- Fernando Stuart, PhD, Postdoc (microbiome)
- Rachel Eddy, PhD. Postdoc (imaging)
- Anthony Tam, PhD, Postdoc (drug target discovery)
- Mai Tsutsui, MD, PhD, Postdoc (radiofrequency therapy)
- Firoozeh Gerayeli, BSc, Master’s Student (COPD biomarker)
- Ana Hernandez, PhD, Postdoc (genetics)
- Chung Cheung, PhD, Research Associate
- Julia Yang, MSc, Research Technician
- Yolanda Yang, MSc, Bioinformatician
- Annie Li, Biostatistician